
Practitioner Seed # 13- Learn your timelines
Imagine you are embarking on a road trip for the holidays….
You must pre-plan your trip
Choose your destination, map your route & calculate an ETA….
Open up google maps, drop your pin at the destination &…….. VOILA!
Now if we ignore the time space continuum, jump in our time machine and head back 20 years, things weren’t so easy!
You would have to pull out the Melways from the back seat (huh? whats a Melways?) in a flurry of pages and piece together a map that feels like your decoding Egyptian hieroglyphics!
This is what it feels like trying to predict an injury timeframe for your patient when you are a new clinician, we know, we have been there!
How can you possibly forecast how long it might take to get your patient back to their training program?
On a background of limited clinical knowledge and diagnostic intuition, the ability to give your patient a clear plan is in its infancy. Often, we have to go back to our clinical mentors to help us determine a timeline for your patient. Over time you will build up your internal pattern recognition on how long an injury might take.
But in the short term, we suggest reading this blog post and get you up to speed with a general framework that you might apply with your patients in the clinic.
Here are some key questions that you can ask yourself upon reflection with a rehab patient……
-
How long has this injury been present
The level of discomfort that people will endure before they bite the bullet and make an appointment to see us, varies greatly. You will see your ‘warrior’ patients who will repeatedly sustain battles with their body and its not until they are on the brink of death, that they come to see you!
It is these patients who start to develop layers of compensations and strategies from a Neuromuscular perspective.
The classic example of this is arthrogenic muscle inhibition (AMI) that occurs predominantly in the quadriceps in the presence of a knee joint effusion (Pietrosimone et al, 2012). Studies have been conducted that involve injection of saline solution into an otherwise healthy knee joint, creating pain & simulating an effusion. (Hodges et al, 2009).
The observed effect = reduced quadricep activity during stair ascent.
So, the human body has an inbuilt tissue preservation system, if it senses danger ie joint injury, it effectively short circuits electrical activity in the area to protect it.
Imagine persistent pain that has been ongoing for months or even years…….
Layers upon layers of compensations, starting with reduced CNS drive, causing decreased peripheral motor unit recruitment & finally, localised tissue atrophy.
Another common phenomenon in people with long term pain …… If you review their scans (Dont worry they will have a whole stack for you!) , you might notice the report highlighting fatty infiltrates within the muscle belly that has undergone atrophy. There are plenty of studies finding fatty infiltrates in deep multifidus in the presence of chronic neck or LBP, similar with longstanding supraspinatus pathology.
2. Is this a case of issues in the tissues?
This is where things can be a little simpler!
Fortunately, we have strong industry knowledge, with occasional scientific support, that certain injuries take a certain amount of time to heal. The caveat here is that there is not one size fits all! Consider the injury mechanism, clinical assessment, characteristics of the individual, sub-acute response, Imaging findings, and you will understand that injury prognosis is very individualised and fluid in nature. Heeding this, as a new graduate, you must start somewhere!
If we come at this from a soft tissue injury perspective…. Lets use the example of a calf injury, maybe soleus as this is the muscle that is injured 70% of the time in the sporting domain:
Soleus injury
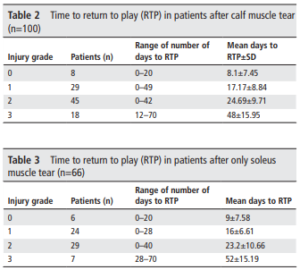
Adapted from Entwistle et al, 2018
If we consider a ligament injury, say an MCL of the knee
Grade 1 – 1-3 weeks
Grade 2 – 4-6 weeks
Grade 3 8-12 weeks
3. What is the pain driver?
The age of pain sciences has taught us that pain is not always as it seems, especially when you’re dealing with long term pain. The once simple feedback loop of :
Noxious stimulus = Nociception = Pain Response
Has now been joined by a plethora of various psychological, cognitive, neuro- endocrine & societal factors that contribute toward the pain experience. If we accept that most tissue of the body will heal within a 6-12 week window (Omitting consolidation of complex stress fractures and surgical reconstructions), then we might expect that as we move farther away from this timepoint, the likelihood of centrally mediated pain escalates.
In this cohort we must base our timeframes around the principles of graded exposure and meeting certain milestones. in this way you can ‘Mini-block” your rehab phases around this criteria. Focus on function over
It has been encouraging to see our industry move toward a more scientific approach to injury rehabilitation. It’s critical that we emphasize the importance of criteria-based progressions. From this perspective, the timeframe is largely dependent on when your patient can achieve the required milestone to exit and progress to the next phase. This relies on an assortment of factors including patient compliance, genetics & environmental factors, to just names a few.
The classic example is that of an ACL injury in an amateur athlete. The rate at which they progress, and are ultimately ready for RTS, will be dependent on how hard they are willing to work, and how they can logistically fit rehab into their work schedule.
While we are ALWAYS criteria based, the patient sitting across from you in the initial appointment will no doubt throw a curly question your way..
How long is this going to take?
At least now, you might have a framework of reference to be able to come back to your patient at appointment 2 or 3 once you have “Gathered all of the necessary information”, and help get them on the path back to optimal health!
Reference:
Pietrosimone BG, McLeod MM, Lepley AS. A theoretical framework for understanding neuromuscular response to lower extremity joint injury. Sports Health. 2012 Jan;4(1):31-5.
Hodges PW, Mellor R, Crossley K, Bennell K. Pain induced by injection of hypertonic saline into the infrapatellar fat pad and effect on coordination of the quadriceps muscles. Arthritis Rheum. 2009 Jan 15;61(1):70-7.

This Post Has 0 Comments